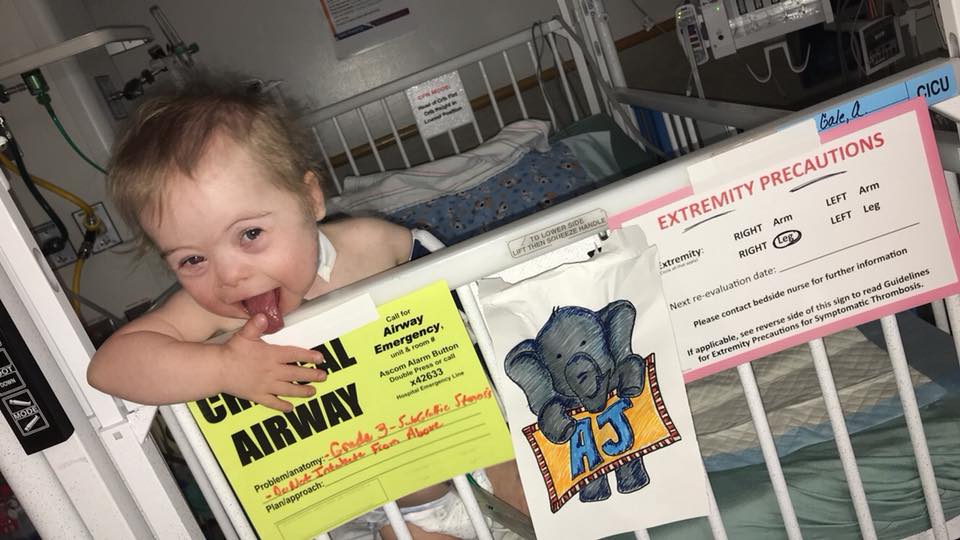
This might get a little technical… so bear with me. I’ll put the cute kid pictures first to try to distract from the details 😉
AJ has a critical airway. That means if his trach comes out he can’t breath and you cant even try to get a new breathing tube in from above. There are lots of people with trachs that can breathe without their trach in – even just for a short while. They may have them for various reasons – in AJs case he has what’s called subglottic stenosis. Which are fancy words for “scar tissue that make it so I can’t breathe”.

The diagram below maps that out a little — above where his trach is, and below his vocal chords is where his problem lies. We’ve had scopes in the past where the docs weren’t able to tell if his vocal chords were paralyzed or not as well due to how much scar tissue there is in that area.

We have known at minimum that AJ would likely need his airway reconstructed – the scar tissue needs to be removed and the airway will need a graft (they use cartilage from his rib) to keep it opened up. We also knew that he was previously classified as having Grade III stenosis (meaning his airway was 71-99% blocked).
What we needed to know was if there was anything in the way of completing this. If AJ isn’t able to manage his secretions (spit/snot 😜), repairing his airway could result in him basically drowning himself. If he has major issues with reflux, trying to do a surgery would cause more harm than good. If there are more upper airway issues than we could see it would complicate things as well. And we also needed to make sure his lungs could support it and the stent they put in his pulmonary artery back in January wasn’t going to cause issues.
Thursday was a whirlwind of doctors and nurses in the airway program at CHOP. Everyone came into the same room, got information from us, and met AJ. It was almost overwhelming. Especially since we had only his Philadelphia at 2 AM and were in the office there at 8 AM. We met with ENT, Pulmonology, GI and Anesthesia and received our instructions for meds and food for the next 24 hours or so. I was up giving meds and food at 11 PM, 1 AM and 430 AM.
We were back in the office at 730 AM on Friday and AJ was hauled off to the OR sometime after 9. The procedure and the transport took roughly an hour before the docs came out to start talking to us.
ENT was first. AJ is still Grade III – which is good as there was concern he could have advanced to IV. He doesn’t have any major airway collapse above or below his trach (we were expecting it to be there!) and his vocal chords are NOT paralyzed! They are scarred, but all things considered it was good news.

They didn’t see any major signs of damage from reflux – which is amazing considering how much he used to throw up. I attached some pictures of AJs scope for reference.
Pulmonology confirmed that the stent that was placed looked good and echoed most of what ENT said.
He also commented that there was fluid in AJs lungs — but that it seemed to all be clear. They did grab some to run labs on to determine if he has chronic bronchitis or anything along those lines.
He has very little space at the top of his carina (where your airway branches off to your lungs) so there is no change needed to his trach size.
They did warn us that our GI doc was going to have some observations for us when she came back up, which she did. AJs digestive tract was pretty red, swollen and angry. There was commentary made about it possibly being H Pylori, but we won’t know and can’t do anything about it until lab results are back. It’s a relatively common GI bug and can be treated but may take a while.
This didn’t really come as a surprise since AJ has been battling stomach issues for a while, and the blended diet we put him on likely helped due to some of the foods we had chosen.
GI also placed a probe that was left in for a day that was used to measure reflux to determine if there are any concerns that need to be controlled there. AJ yanked it out 30 minutes before the study was up, but GI confirmed they had enough data so we didn’t have to have it replaced.
We don’t have a final verdict as there are still lab results out – waiting for the probe results, cultures and biopsies, but the short story is that he’s most likely eligible for repair.
BUT… There’s always a but.
The airway repair he needs requires a graft. Dr Jacobs (ENT) was confident he could make AJs airway look great on a table, but he’s concerned that AJs lower oxygen saturations would make it difficult for the graft to heal correctly.
So now our ENT gets to discuss with our Cardiac Surgeon to determine what comes next – the next heart repair (which will increase his oxygen saturations but also comes with risks due to the way his blood flow works), or his airway repair (which will come with the risk of not lasting.)
The joke in the room at this point was that doing the surgery would be the easy part compared to trying to get to a consensus.
End of next week we call in for lab results from pulmonology and GI so we can work out our next steps there, and next month Dr Jacobs (ENT) and Dr Gaynor (Cardiac Surgeon) will be meeting to discuss what’s next.
Until then? We’re on the road home, exhausted and in need of a full day of sleep, but happy with what we were able to accomplish.
So very thankful for the team of doctors who pour their hearts into these kids every single day. And for the chance to be a CHOP family – we love our UIHC family too – but there’s something inspiring about being able to go out to CHOP and almost every elevator ride finding out that you’re in the presence of another family with complex issues. Sitting in a waiting room with kids who have had their trach removed recently, who are helping their parents kick on their feeding tubes, listening to other parents grumble at their suction machines and silencing alarms…. it truly helps knowing that we’re not alone and that we are in the right place with the right people. 💕